Diabetes
The Definition
- Diabetes mellitus refers to a group of diseases that affect how your body uses blood sugar (glucose).
- Glucose is vital to your health because it’s an important source of energy for the cells that make up your muscles and tissues.
- It’s also your brain’s main source of fuel.
- If you have diabetes, no matter what type, it means you have too much glucose in your blood, although the causes may differ.
- Too much glucose can lead to serious health problems.
- Chronic diabetes conditions include type 1 diabetes and type 2 diabetes.
- Potentially reversible diabetes conditions include prediabetes — when your blood sugar levels are higher than normal, but not high enough to be classified as diabetes — and gestational diabetes, which occurs during pregnancy but may resolve after the baby is delivered.
- To understand diabetes, first you must understand how glucose is normally processed in the body.
How Insulin works:
- Insulin is a hormone that comes from a gland situated behind and below the stomach (pancreas).
- The pancreas secretes insulin into the bloodstream.
- The insulin circulates, enabling sugar to enter your cells.
- Insulin lowers the amount of sugar in your bloodstream.
- As your blood sugar level drops, so does the secretion of insulin from your pancreas.
The Role of Glucose:
- Glucose — a sugar — is a source of energy for the cells that make up muscles and other tissues.
- Glucose comes from two major sources: food and your liver.
- Sugar is absorbed into the bloodstream, where it enters cells with the help of insulin.
- Your liver stores and makes glucose.
- When your glucose levels are low, such as when you haven’t eaten in a while, the liver breaks down stored glycogen into glucose to keep your glucose level within a normal range.
The Causes
Diabetes Type 1:
- The exact cause of type 1 diabetes is unknown.
- What is known is that your immune system — which normally fights harmful bacteria or viruses — attacks and destroys your insulin-producing cells in the pancreas. This leaves you with little or no insulin.
- Instead of being transported into your cells, sugar builds up in your bloodstream.
- Type 1 is thought to be caused by a combination of genetic susceptibility and environmental factors, though exactly what many of those factors are is still unclear.
Prediabetes & Type 2:
- In prediabetes — which can lead to type 2 diabetes — and in type 2 diabetes, your cells become resistant to the action of insulin, and your pancreas is unable to make enough insulin to overcome this resistance.
- Instead of moving into your cells where it’s needed for energy, sugar builds up in your bloodstream.
- Exactly why this happens is uncertain, although it’s believed that genetic and environmental factors play a role in the development of type 2 diabetes.
- Being overweight is strongly linked to the development of type 2 diabetes, but not everyone with type 2 is overweight.
Gestational Diabetes:
- During pregnancy, the placenta produces hormones to sustain your pregnancy.
- These hormones make your cells more resistant to insulin.
- Normally, your pancreas responds by producing enough extra insulin to overcome this resistance.
- But sometimes your pancreas can’t keep up.
- When this happens, too little glucose gets into your cells and too much stays in your blood, resulting in gestational diabetes.
The Complications
- Long-term complications of diabetes develop gradually. The longer you have diabetes — and the less controlled your blood sugar — the higher the risk of complications.
- Eventually, diabetes complications may be disabling or even life-threatening.
- Possible complications include:
- Cardiovascular disease. Diabetes dramatically increases the risk of various cardiovascular problems, including coronary artery disease with chest pain (angina), heart attack, stroke and narrowing of arteries (atherosclerosis).
- If you have diabetes, you are more likely to have heart disease or stroke.
- Nerve damage (neuropathy).
- Excess sugar can injure the walls of the tiny blood vessels (capillaries) that nourish your nerves, especially in your legs.
- This can cause tingling, numbness, burning or pain that usually begins at the tips of the toes or fingers and gradually spreads upward.
- Left untreated, you could lose all sense of feeling in the affected limbs.
- Damage to the nerves related to digestion can cause problems with nausea, vomiting, diarrhea or constipation.
- For men, it may lead to erectile dysfunction.
- Kidney damage (nephropathy).
- The kidneys contain millions of tiny blood vessel clusters (glomeruli) that filter waste from your blood.
- Diabetes can damage this delicate filtering system.
- Severe damage can lead to kidney failure or irreversible end-stage kidney disease, which may require dialysis or a kidney transplant.
- Eye damage (retinopathy).
- Diabetes can damage the blood vessels of the retina (diabetic retinopathy), potentially leading to blindness.
- Diabetes also increases the risk of other serious vision conditions, such as cataracts and glaucoma.
- Foot damage.
- Nerve damage in the feet or poor blood flow to the feet increases the risk of various foot complications.
- Left untreated, cuts and blisters can develop serious infections, which often heal poorly.
- These infections may ultimately require toe, foot or leg amputation.
- Skin conditions.
- Diabetes may leave you more susceptible to skin problems, including bacterial and fungal infections.
- Hearing impairment.
- Hearing problems are more common in people with diabetes.
- Alzheimer’s disease.
- Type 2 diabetes may increase the risk of Alzheimer’s disease.
- The poorer your blood sugar control, the greater the risk appears to be.
- Although there are theories as to how these disorders might be connected, none has yet been proved.
- Complications of gestational diabetes.
- Most women who have gestational diabetes deliver healthy babies.
- However, untreated or uncontrolled blood sugar levels can cause problems for you and your baby.
- Cardiovascular disease. Diabetes dramatically increases the risk of various cardiovascular problems, including coronary artery disease with chest pain (angina), heart attack, stroke and narrowing of arteries (atherosclerosis).
Obesity & Diabetes
- Obesity and type 2 diabetes are metabolic disorders that have strong associations with body composition.
- The metabolic perturbations that characterize type 2, those of:
- hyperglycemia,
- elevated fasting insulin,
- increased fatty acids and triglycerides,
- and, most fundamentally, insulin resistance,
- have been found to be associated with adiposity and perhaps, more particularly, with certain patterns of adipose tissue and fat distribution.
- Insulin resistance is a principal mechanism by which obesity is considered to heighten risk of type 2 diabetes.
- In obesity, there is insulin resistance in adipose tissue and muscle.
- Weight change (gain vs. loss or stabilization) has been found to influence risk for development of type 2 diabetes in both men and women.
- In several investigations of older adults, including large population studies, neither the amount of fat-free mass nor the amount of skeletal muscle was associated with insulin resistance or type 2 diabetes.
- Obese individuals are insulin resistant after adjustment for fat-free mass.
- However, the quality rather than the quantity of fat-free mass has been found to be a very important body composition consideration in insulin resistance, obesity, and type 2 diabetes.
The Effects of Weight Loss
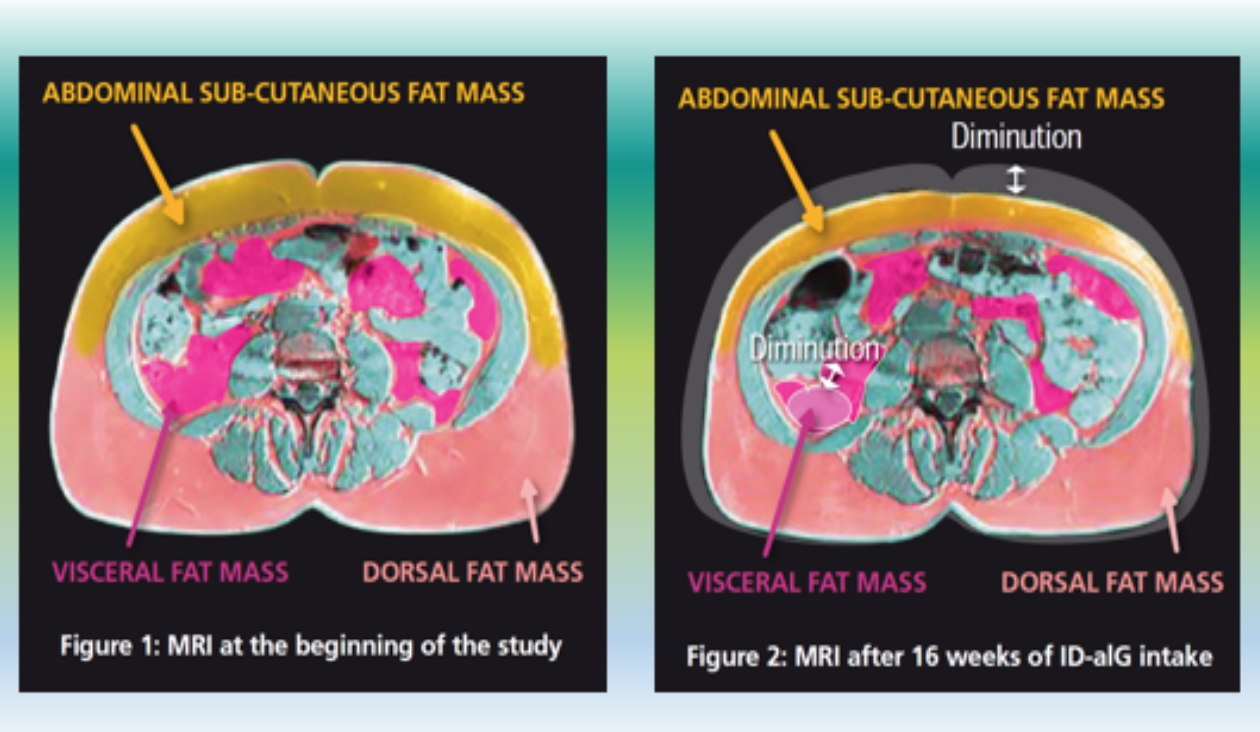
- During the past 3 decades, perhaps the single most important advance in linking body composition research to a more complete understanding of type 2 diabetes and of insulin resistance in general has been attained through measurements of visceral adipose tissue (VAT).
- The association between VAT and Insulin Resistance is also observed in those without type 2 diabetes and exists with general consistency across sex, race, and a variety of other subgroups of the population.
- Interestingly, this relationship is also observed among normal-weight men and women.
Health ABC Study
- When BMI criteria were used to appraise obesity in a large-scale cohort of more than 3,000 men and women in the Health, Aging and Body Composition study, VAT was found to be a strong predictor of insulin resistance and type 2 diabetes, particularly among nonobese people.
- This suggests that older adults can be at greater risk for the development of type 2 diabetes if they have excess VAT.
- VAT is a strong predictor of insulin resistance and type 2 diabetes in children and adolescents, a segment of the population also becoming more obese.
- With regard to those who already have type 2 diabetes, modest weight loss of 5% to 10% can have a pronounced effect in improving hyperglycemia and reducing other cardiovascular risk factors.
- Similar amounts of weight loss substantially reduce the risk for development of type 2 diabetes.
- Insulin resistance and hyperglycemia can begin to improve rapidly once a patient with type 2 diabetes begins weight loss.
- Indeed, it seems that these improvements almost precede weight loss.
- Somewhat surprisingly, in patients with type 2 diabetes, the improvements in hyperglycemia do not seem to be highly correlated with the amount of weight loss or amount of change in regional adiposity.
- In a recent weight loss intervention study in type 2 diabetes, the improvements in hyperglycemia were significantly correlated with improved insulin sensitivity but not with weight loss per se or specific changes in regional adiposity.
- For example, in a weight loss study, we observed that among obese nondiabetic participants, the percentage decrease in visceral fat was the only body composition change that significantly predicted the improvement in insulin resistance after weight loss.

The Medical Cost Savings
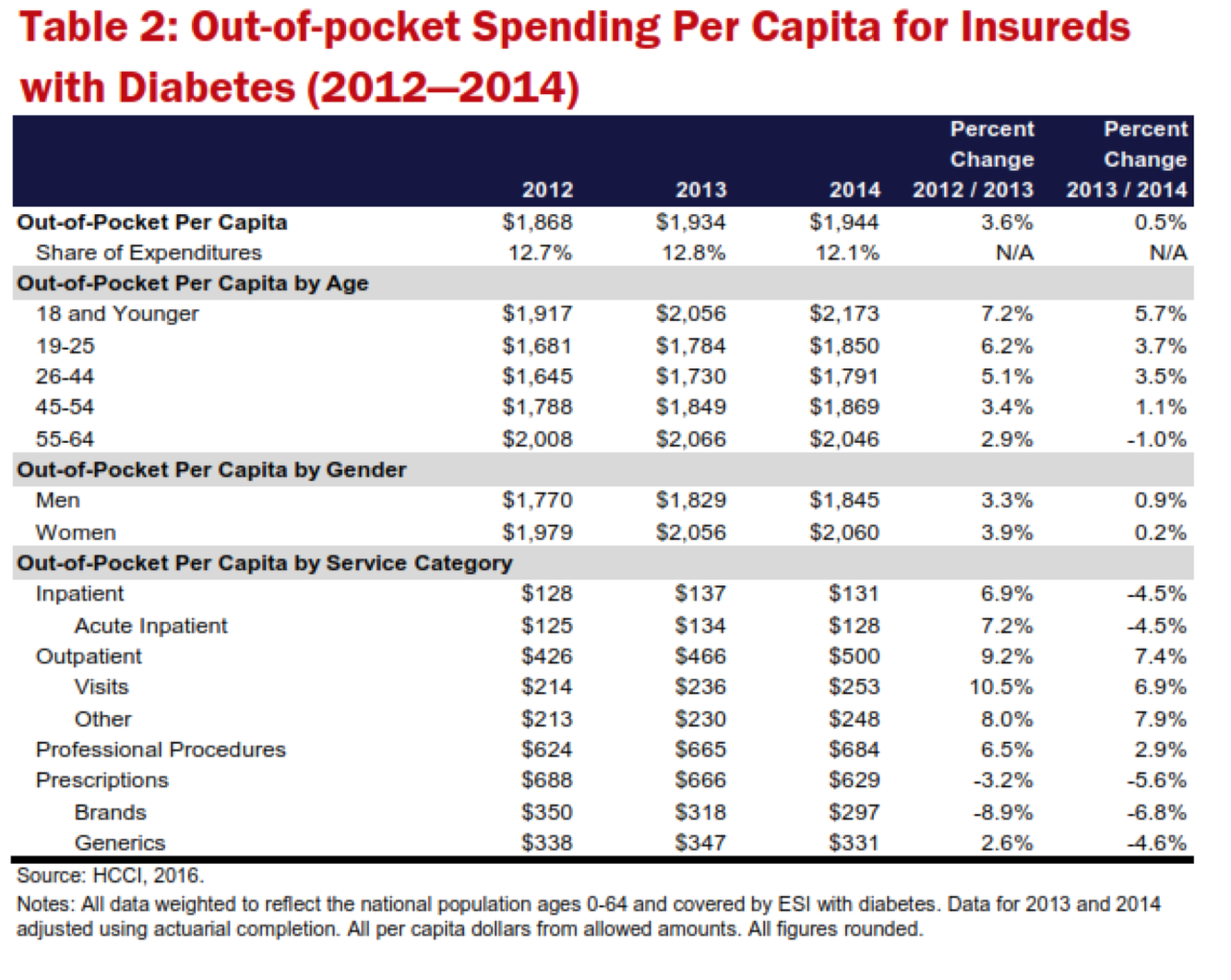
- The American Diabetes Association (ADA) estimated that for the entire population of Americans with diagnosed diabetes in 2012, per capita spending on health care was $13,741.
- For that year (the most recent year that per capita health care spending estimates were available from the ADA), they found that per capita spending for people with diabetes was 3.9 times higher than spending for people without diabetes.
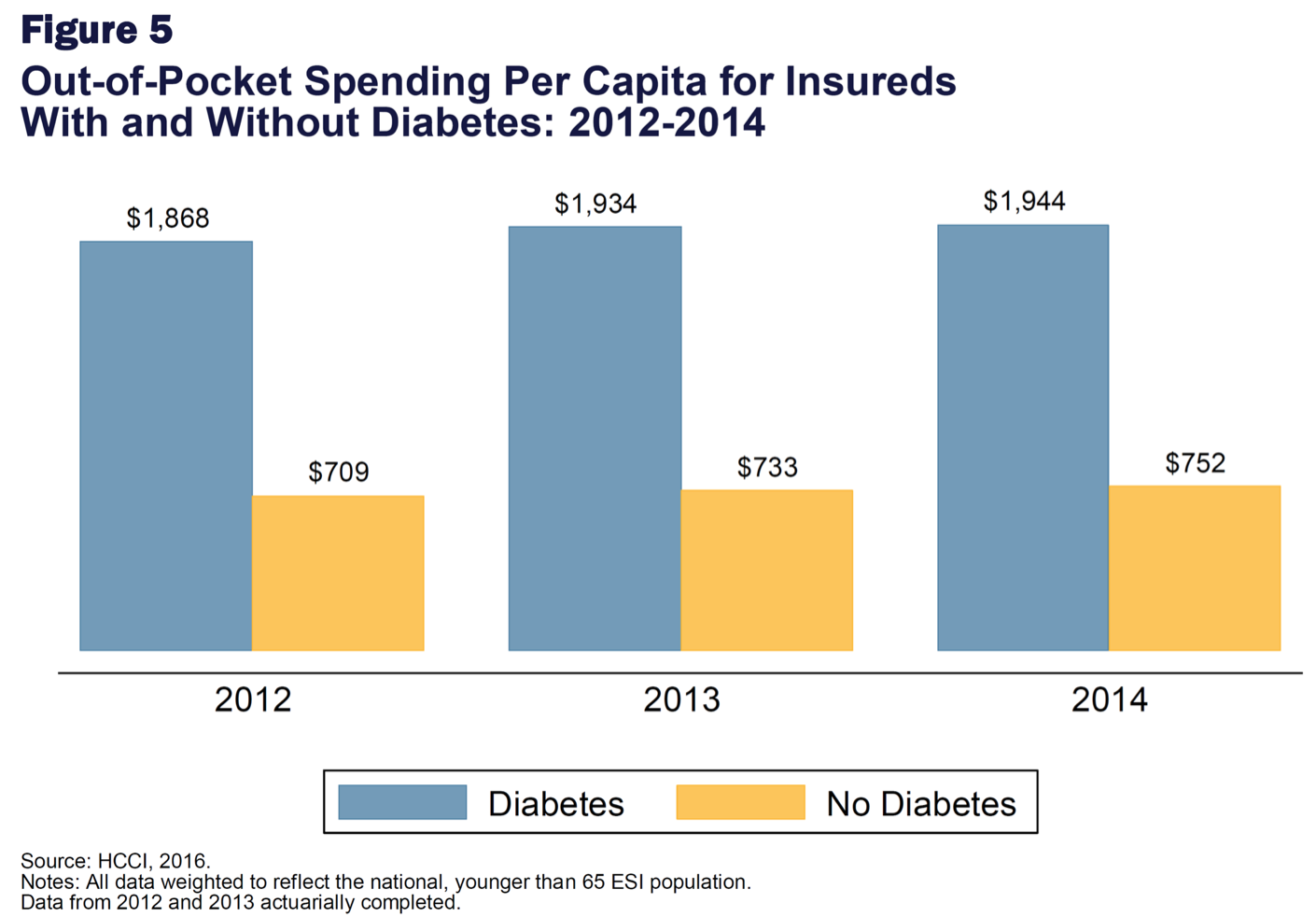
- In 2014, out-of-pocket spending per capita for people without diabetes was $752, increasing by $43 per person over the study years.
- In 2014, people with diabetes spent $1,944 out of pocket per capita.
- Of total per capita spending on health care in 2014 ($16,021), 12.1% was spent out of pocket by people with diabetes according to the 2014 Diabetes Health Care Cost and Utilization Report (Source NCCI).
- Out-of-pocket Cost Difference: $1,192